When a patient hands over their insurance card or uses the hospital’s patient portal to make the necessary payments, no matter if it’s keyed in or contactless, the process generates data that can expose personal details if misused.
That risk is why the United States enacted the Health Insurance Portability and Accountability Act of 1996 — HIPAA. Its objective is twofold: to keep medical coverage portable across employers and to defend the privacy and security of health information. For clinics, insurers, and the rising sector of cloud vendors, compliance is more than a regulatory checkbox; it is a trust agreement with every patient whose record passes through their servers.
This beginner’s guide covers HIPAA’s framework, goes over its standards, the actors who must comply, and the practical steps every company can take to protect patient data privacy while avoiding hefty penalties. Services like medical record scanning are important for maintaining HIPAA compliance for both covered entities and business associates. Our guide on medical record scanning explains how digitizing records enhances productivity, ensures HIPAA compliance with secure storage and encryption, and transforms healthcare practices for better patient care.
The Five Titles of HIPAA
HIPAA compliance stands on five Titles. Each title tackles a different administrative problem in health care. Here’s a look at each:
| Title | Focus | Practical Impact on Data Management |
| I – Health Insurance Reform | Protects those with pre-existing conditions and assures renewability of group plans | Drives need for reliable enrollment records and error-free data interchange between employers and insurance. |
| II – Administrative Simplification | Establishes nationwide rules for handling electronic health records and requires measures to keep patient information secure. | Spawned the Privacy, Security, Breach Notification, and Enforcement Rules that IT and compliance teams follow daily. |
| III – Tax-Related Health Provisions | Allows tax deductions for medical insurance and medical savings accounts | Employers must store contribution records securely because they still contain PHI. |
| IV – Group Health Plan Reforms | Further limits coverage exclusions and clarifies COBRA continuation | Health plans exchange eligibility files that must meet HIPAA transaction standards. |
| V – Revenue Offsets | Sets rules for company-owned life insurance and recoups enforcement costs | Less visible to clinicians, but payroll vendors handling these benefits become business associates under Title II. |
Who Must Follow HIPAA?
HIPAA names two broad classes of regulated parties: covered entities and business associates.
- Covered entities are organizations like doctors, clinics, insurance companies, and billing services that handle patient data electronically for things like claims and payments. Doctors’ offices, pharmacies, dentists, and large hospital systems all fall here.
- Business associates are third-party vendors that handle patient information for a covered entity, whether they collect it, store it, send it, or use it in some way. These “covered entities” can be billing companies, cloud hosting firms, IT consultants, shredding services, and yes, document scanning services that turn paper charts into indexed PDFs.
Both groups sign Business Associate Agreements (BAAs) spelling out how they will safeguard data and what happens if a breach occurs. Failing to execute a BAA is itself a violation.
Key Provisions Every Beginner Should Know
Here are some key provisions you should know:
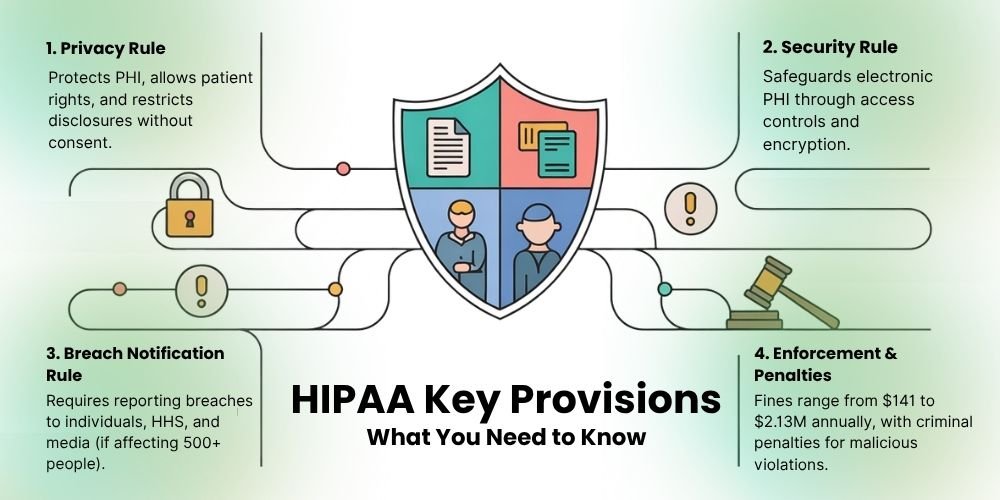
1. Privacy Rule
The Privacy Rule defines PHI and gives patients the right to access, amend, and receive an accounting of their records. It limits how covered entities may use or disclose data without written consent – for example, sharing with another treating provider is allowed, but releasing information to a marketer is not.
2. Security Rule
The Privacy Rule applies to both paper and electronic health records, but the Security Rule focuses only on electronic ones. It says that healthcare providers must set up safety steps—like giving access only to the right people, using unique user IDs, and keeping doors to data areas locked—to protect patients’ electronic information. Encryption is “addressable,” meaning organizations must use it or document why an alternative offers equal protection.
3. Breach Notification Rule
If a breach of unsecured PHI occurs, covered entities must notify affected individuals within 60 days and the Department of Health & Human Services (HHS). Large breaches affecting 500 or more people also trigger a media notice.
4. Enforcement Rule and Penalties
HIPAA is enforced by the Office for Civil Rights (OCR). The four tiers of civil monetary fines under HIPAA depend on negligence levels, which result in annual penalties ranging from $141 to $2.13 million per infraction category. These amounts are adjusted annually for inflation; check the HHS website for the most current numbers. The OCR has collected $145 million through 152 settlements to date.
Oregon Health & Science University received a $200,000 penalty from OCR in December 2024 for multiple violations. The penalties for criminal violations include monetary fines, together with possible jail time when PHI violations are committed with malicious intent to sell or use PHI.
Why HIPAA Matters for Patient Data Privacy?
The adoption of electronic records speeds up care delivery while improving coordination between providers, yet introduces additional security vulnerabilities through cloud servers and laptops and mobile applications, and external consultant access. Under HIPAA, patients can trust that their ICD codes, together with test results and insurance details, remain protected from unauthorized disclosure or sale regardless of technological advancements. The strict standards help providers maintain superior cybersecurity practices and prevent expensive system downtime.
HIPAA has motivated the development of new healthcare solutions because medical record scanning vendors now provide chain-of-custody tracking, and healthcare data security solutions offer audit trails with real-time anomaly warnings. HIPAA establishes minimum standards that drive the market toward developing products that protect lives at the same level as medical drugs and implants.
Simple Steps For Easy HIPAA Compliance

You do not need a legal degree to start good practice. Follow these core actions:
- Conduct a risk analysis – First, get to know where ePHI is stored, processed, and transmitted. Prioritize high-risk gaps such as unencrypted laptops.
- Create written policies – In this policy, you should cover access control, media disposal, workstation use, and incident response. Update yearly.
- Train every staff member – Anyone newly hired should be trained before they have access to any patient information. After the initial training, all staff should go through updated training once a year.
- Secure systems – Implement unique logins, strong passwords, time-out screens, and patches. Encrypt data at rest and in transit.
- Use Business Associate Agreements – Sign a BAA with any vendor that handles PHI, including document scanning services.
- Maintain audit logs – Record who accessed which record and when. Retain logs for at least six years.
- Plan for contingencies – Back up data off-site, test restoration, and keep an emergency mode operations plan.
- Run regular audits – Internal or third-party reviews catch policy drift and prove due diligence during OCR investigations.
- Document everything – If it is not documented, regulators treat it as if it never happened.
These measures satisfy many Security Rule implementation specifications and show good-faith effort if an incident arises.
How Modern Image Helps You Stay Compliant
Paper charts and legacy files are still common in specialty practices and rural clinics. Scanning them to a secure digital format reduces storage costs and makes retrieval faster, yet the conversion itself introduces risk. Modern Image solves that problem by offering medical record scanning and indexing in a HIPAA-qualified facility. Key safeguards include:
- Locked chain-of-custody bins for transport
- Background-checked technicians who work in badge-restricted zones
- Production-grade scanners that erase images from internal memory after each batch
- Encrypted file delivery through a client portal with time-limited links
- Destruction certificates for shredded originals when required
Modern Image can also integrate with your EHR or cloud storage so the scanned files inherit existing permissions, supporting a layered healthcare data security posture. If your office needs to respond to an OCR data request, the indexed PDFs speed retrieval and reduce stress.
Conclusion
HIPAA may sound like a “hard to achieve” standard at first, but its underlying principle is simple: every patient deserves control over who sees their health information, and every institution that handles that data must secure it. Understanding the standard’s five Titles, recognizing if you are a covered entity or business associate, and implementing the Privacy and Security Rules offers you a clear route. Start with staff education, secure passwords, and documented procedures, then check progress with monthly audits.
Whether you are a lone physician scanning decades of paper charts or a regional clinic replacing servers, compliance scales with your effort. Partnering with service businesses that understand HIPAA, such as Modern Image for secure document scanning services, allows your staff to focus on care while specialists manage conversion and protection.
So, contact the professionals and make your practice HIPAA compliant.